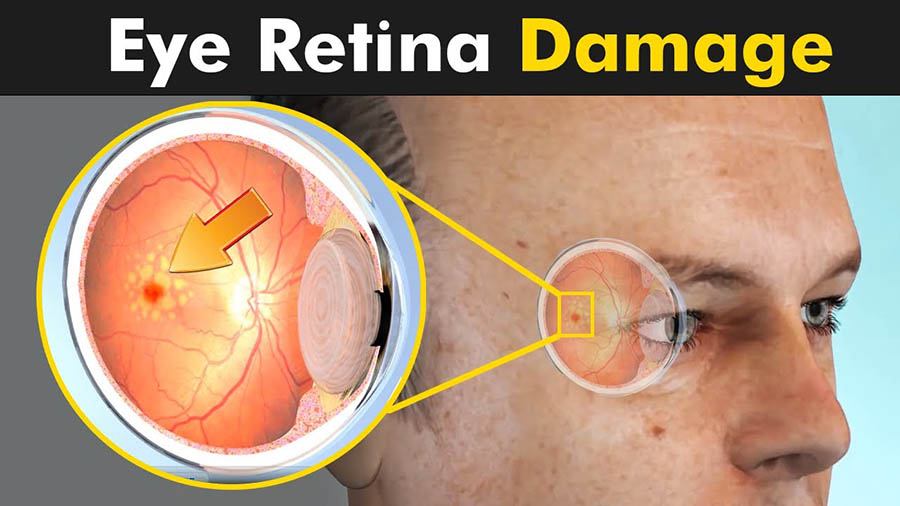
Retina is a light-sensitive lining in the back of the eye. It contains millions of special nerve cells that react to light. These photoreceptors send electrical impulses to the optic nerve, which your brain converts into https://katariahospital.com/images which we see. In the center of this nerve tissue is the macula. It provides the sharp, central vision needed for reading, driving and seeing fine detail.
Retinal disorders affect this vital tissue. They can affect your vision, and some can be serious enough to cause blindness. Most commonly seen are-
- Macular degeneration – a disease that destroys your sharp, central vision
- Diabetic eye disease
- Retinal detachment – a medical emergency, when the retina is pulled away from the back of the eye
- Retinoblastoma – cancer of the retina. It is most common in young children.
- Macular pucker – scar tissue on the macula
- Macular hole – a small break in the macula that usually happens to people over 60
- Floaters – cobwebs or specks in your field of visionWhat Kataria Eye & ENT Hospital Pvt. Ltd. offers?
Thorough evaluation and accurate diagnosis is critical to receiving the most appropriate treatment. At Kataria Eye & ENT Hospital, we offer the most State of the art Diagnostic modalities like— OCT (Optical Coherence Tomography),–Fundus Fluoroscein Angiography A technique for examining the retina’s circulation uses a dye tracing method.–Frequency Doubled Green Lasers are available for treatment of all kinds of retinal disorders.What we treat?
Common retinal diseases treated by Kataria EYE & ENT Hospital include-
1. Macular Degeneration – What is AMD?
It is the most common cause of legal blindness in adults. One of several types of macular degeneration, AMD occurs when the small central portion of the retina (the macula) is diseased and the eye’s ability to distinguish fine details is affected. Most patients have the “dry” form, in which yellow deposits (drusen) are present in the macula. Drusen may be asymptomatic or accumulation may cause dimming or distortion. In advanced stages of dry AMD, the disease can cause blind spots and central vision loss.
About 10 percent of AMD patients develop the “wet” form, in which abnormal blood vessels grow from the choroid and under the retina. The vessels leak blood and fluid into the retina, distorting vision (making straight lines look wavy), and creating blind spots and central vision loss.How is AMD treated?
There is no cure for AMD, but early detection and treatment can delay or reduce its severity.
- ANTIOXIDANTS — A combination of vitamins C, E, lutein, zeaxanthin, zinc and copper have been shown to decrease the risk of vision loss in patients with intermediate to advanced dry AMD or wet AMD in one eye.
- ANTIOXIDANTS — A combination of vitamins C, E, lutein, zeaxanthin, zinc and
- ANTI VEGF drugs — Currently used as firstline therapy for wet AMD, the results of clinical trials of local injections of ranibizumab (Lucentis®), afibercept (Eylea®) and bevacizumab (Avastin®) for active wet AMD showed visual stability in about 95 percent of patients and visual gain in about 35 percent of patients.
- PDT — this involves the injection of a light-sensitive drug into the bloodstream. After being absorbed by the abnormal blood vessels, the drug is activated with a cold laser, which destroys the unwanted blood vessels in select wet AMD cases.
- Laser therapy — High-energy light is occasionally used for select subtypes of wet AMD to destroy active growing abnormal blood vessels.
2. Diabetic Retinopathy
Diabetic retinopathy occurs when diabetes damages the tiny blood vessels in the retina. In the early stages of the disease (non-proliferative retinopathy), these blood vessels may leak fluid, resulting in edema. In the more advanced stage (proliferative retinopathy), fragile new blood vessels grow in the retina and in the vitreous humor (a clear substance that fills the eye). If left untreated, these blood vessels may bleed and cloud vision, or may scar and detach the retina.
How is diabetic retinopathy treated?
Regular monitoring of the retina with dilated fundus exams and leading-edge imaging technologies (such as optical coherence tomography) is important in diabetic retinopathy. If detected at earlier stages, more than 90 percent of patients can be saved from blindness. Other treatments include:
- Medications — Now becoming the first-line treatment for many types of diabetic eye disease, these medications include anti-vascular endothelial growth factor inhibitors (such as ranibizumab, afibercept and bevacizumab), steroids (such as dexamethasone intravitreal implant, or Ozurdex®), fluocinolone acetonide intravitreal implant (Iluvien®) and triamcinolone acetonide injectable suspension (Triescence®).
Studies show that stability and improvement in visual acuity appearsto be more significant with these therapies. - Laser surgery — In many cases, laser surgery reduces the risk of future vision loss. Laser photocoagulation can be performed to seal or destroy growing or leaking blood vessels in the retina.
- Vitrectomy — In some people with diabetic retinopathy, the blood that leaks from blood vessels in the retina also may leak into the vitreous humour, clouding vision. These vessels also may cause scar tissue and subsequent retinal detachment. Vitrectomy can be used to remove the blood or repair a retinal detachment. Be sure to schedule follow-ups with your primary care physician and/or endocrinologist to optimize systemic control of blood sugar, blood pressure and blood lipids.
3. Retinal Detachment
What is retinal detachment?
Retinal detachment is a serious condition that occurs when the retina pulls away from its supporting tissues. Since the retina cannot work properly under these conditions, permanent vision loss can occur if a detachment is not repaired quickly.
Nearsightedness, previous trauma, family history of retinal detachment and previous eye surgery increase risk for retinal detachment, but it may also be spontaneous.How is retinal detachment treated?
There are a number of approaches to treating a detached retina, including:
- Laser (thermal) or freezing (cryopexy) — If diagnosed early enough, both of these approaches can repair a retinal tear before it causes retinal detachment.
- Pneumatic retinopexy — Repairs select retinal detachments. Cryo treatment is first used to seal the tear. A small gas bubble is injected into the vitreous, where it rises and presses against the retina, closing the tear.
- Scleral buckle — this procedure involves placing a silicone band (buckle) around the eye to hold the retina in place. This band is not visible and remains permanently attached. Cryo treatment closes the tear. A gas bubble is often used to help reattach the retina.
- Vitrectomy — Used for large tears, the vitreous is removed from the eye and replaced with a saline solution. A gas or silicone oil bubble and laser are used at the time of vitrectomy to facilitate repair. Patients will need to maintain a face-down position for a period of time to keep the bubble in place .Success rates are similar to the scleral buckle. In some cases, both scleral buckle and vitrectomy are indicated to repair a retinal detachment.




